1. BLAST (Basic Local Alignment Search Tool)
Interface: Web and command-line
Immune‑gene use: Rapidly identifies homologs of immune-related genes (e.g., cytokines, T‑cell receptor chains) by alignment to annotated databases. Gold standard for sequence similarity searches bversity.io.
2. Galaxy
Interface: Intuitive GUI, no-code workflows, cloud ready bversity.io
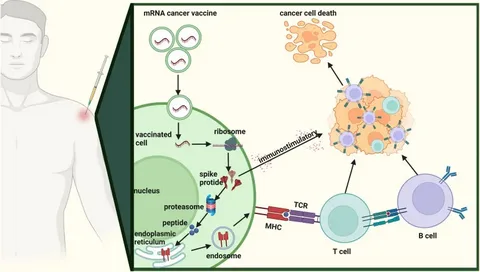
Immune‑gene use: Build reproducible RNA‑seq and ChIP‑seq pipelines for profiling immunoreceptor expression, immune signaling pathway activity, epitope mapping, and metadata integration.
3. Bioconductor (R)
Interface: R packages, GUI via RStudio
Immune‑gene use: DESeq2, edgeR, immunedeconv, flowCore: differential mRNA of cytokines, deconvolution of immune‑cell populations; variant annotation in immune‑related loci immunology.hms.harvard.edu.
4. ShinyGO
Interface: Web‑based R Shiny
Immune‑gene use: Gene-set enrichment on immune gene lists; overlays genes onto KEGG/Reactome immune pathways like TLR, antigen processing reactome.org.
5. Metascape
Interface: Web portal
Immune‑gene use: Multi-list enrichment & PPI networks for immune clusters; integrates GO, Reactome, MSigDB immune modules.
6. Reactome Analysis Tools
Interface: Web mapping/enrichment & Cytoscape ReactomeFIViz plugin
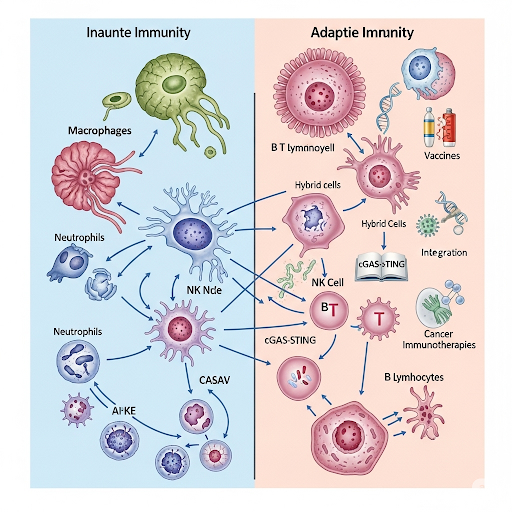
Immune‑gene use: Map expression variants in innate/adaptive pathways; overlay miRNA or cytokine transcript changes onto pathway diagrams.
7. GeneXplain Platform
Interface: Web browser GUI, drag‑and‑drop bricks
Immune‑gene use: TFBS prediction (e.g., NF‑κB, STATs), analyze ChIP‑seq on promoter regions of immune genes, build end‑to‑end workflows.
8. OLAF (Open Life Science Analysis Framework)
Interface: Conversational LLM‑based web UI
Immune‑gene use: Natural‑language workflows for single‑cell RNA‑seq focusing on immune cell clusters, marker gene annotation, pathway visualization — ideal for non‑bioinformaticians.
9. SnapGene Viewer
Interface: Desktop/online GUI
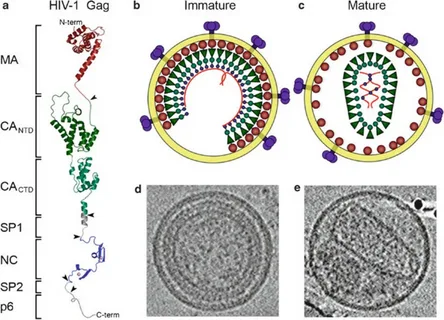
Immune‑gene use: Visualize and annotate plasmids for immune gene cloning (e.g., IL‑genes, TCR constructs); simulate primer design for gene editing.
10. EBI Search / EMBL‑EBI Tools
Interface: Web portal + REST API
Immune‑gene use: Comprehensive search across AlphaFold structures, domain databases, expression atlas; ideal for retrieving variant info and structural data for immune receptors.
🧬 Why These Are Ideal for Immune Research
| Feature | Examples |
|---|---|
| GUI + pipelines | Galaxy, GeneXplain, OLAF support no-code workflows |
| Gene/pathway-focused | ShinyGO, Metascape, Reactome map immune-specific gene sets |
| Deep annotation | Bioconductor enables statistical modeling, EBI and Reactome support structure and pathway analysis |
| Cloning & design | SnapGene aids in construct visualization, primer design for immune genes like cytokines |
🔧 Integration Tips
- Start with Galaxy workflows for QC → alignment → differential expression on immune cell datasets
- Use Bioconductor in RStudio to analyze immune gene expression patterns and cell-type deconvolution
- Analyze gene lists with ShinyGO & Metascape to validate enrichment in immune pathways
- Dive deeper with Reactome, linking DE genes to pathway maps
- Finalize with SnapGene/EBI for cloning, structural prediction, and variant annotation